According to two recent studies, men who have surgery to create a new penis appear to have good long-term outcomes. The majority of patients undergoing the phalloplasty procedure are transgender men who wish to have a surgical transition. However, men who have lost their penis due to trauma or cancer, including wounded soldiers, can also consider this option.
Both patient groups were included in the new studies, which will be presented on Saturday at the annual meeting of the American Urological Association in San Diego. Furthermore, the research indicates that both kinds of patients generally have positive long-term outcomes.
“Many individuals might not be aware that there are physicians with this ability,” stated Dr. Gregory Bales, a University of Chicago surgeon and urologist who was not involved in the research.
However, according to Bales, an AUA spokesman who will moderate these meeting presentations, the procedure can be “life-altering,” for both transgender men and those who have lost their penis in an accident or other trauma. In one of the studies, ten men who had undergone phalloplasty following a traumatic loss of penis—most often from a blast injury or car accident—were followed by British researchers at University College London.
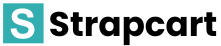
In each instance, the surgeons created a new penis using skin and other forearm tissue. According to Bales, that procedure, called radial artery-based forearm phalloplasty, is most likely the most utilized one. According to Dr. Nim Andrew Christopher, a consultant urologist and andrologist who worked on the study, it also usually has the best results.
He explained that this is partly because the forearm has minimal fat, minimal hair, and a sizable nerve and blood vessel that can be removed, along with some soft tissue and skin, to create a penis that feels and looks natural.
The organ is then cautiously affixed to the groin’s blood vessels and nerves. The urethra, the tube that conveys urine and semen through the penis, required total reconstruction for a few of the men in Christopher’s study.
Christopher declared, “It’s not a surgery for the weak of heart.” “It takes multiple procedures, and we don’t always get it just right the first time.”
The researchers report that all three of the study participants who experienced blood clots or a blockage in the new urethra were successfully treated. After an average of slightly more than four years, all of the patients reported being satisfied with the new penis’s size, look, and feel. The men could all urinate in a regular manner as well. “It’s as good as the real thing,” Christopher exclaimed.
A man needs to have an inflatable device implanted in the new penis in order for him to engage in sexual activity following surgery. Bales continued, “Just making the penis is kind of like making a hood ornament.” “It will have no ability for penetrative intercourse without the implant.” In Christopher’s research, six males selected an
implant; three ultimately required revision surgery as a result of an infection or a “mechanical failure.”
According to Bales, the saline-filled devices have the potential to break or “erode” through the skin. Ultimately, he stated, any man who has a penile implant will require another surgery since the devices “don’t last forever.” The second study examined ninety-three patients who, between 1983 and 2015, had undergone phalloplasty at a single hospital in Virginia. In the group were 49 men and 44 transgender patients who had undergone the surgery to address a congenital defect or following trauma.
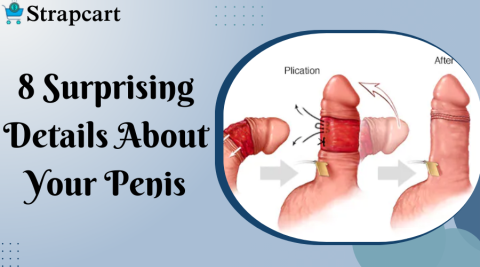
39 percent of transgender men and 48 percent of other men rated their urinary function as “excellent” after an average of 4.5 years. Seventy percent expressed satisfaction with the sensation provided by the new organ, and twenty-five percent reported engaging in sexual activity. Compared to other men, transgender men had a higher risk of developing a blockage in the urethra (56 percent versus 30 percent). Bales says that’s most likely because the urethra is built “from scratch” for patients who identify as transgender.
Other problems may also arise. According to Bales, patients may experience arm numbness or weakness following the procedure, which leaves a scar on the forearm. A practical barrier to obtaining the procedure exists as well. Bales estimated that the procedure is likely performed by only 30 to 40 surgeons in the United States. It might require a lot of patients to travel to get it.
Plans might cover the procedure even though insurance coverage varies; this could be the case, for instance, if a transgender patient has been diagnosed with gender dysphoria, according to Bales. ” The number of surgeries and complications have an impact on the overall cost of the project,” Bales stated. “But it is safe to say that it is well over $100,000 (estimated R1.4 million).”